

- Do telehealth visits have copays update#
- Do telehealth visits have copays upgrade#
- Do telehealth visits have copays full#
- Do telehealth visits have copays free#
An email exchange got the bill reversed, he said. A week earlier and the charge could have caused a bank overdraft, he said. “It happened to be payday for me,” he said. The office charged the whole visit - $280, not just the copay ― to his debit card without notifying him.
Do telehealth visits have copays full#
“So these providers are protecting themselves upfront by either asking for full payment or by getting the copayment.”ĭavid DeKeyser, a marketing strategist in Brooklyn, New York, sought a physician’s advice via video after coming in contact with someone who attended an event where coronavirus was detected. “A lot of providers may not have agreements in place with the plans that they work with to deliver services via telemedicine,” she said.

New rules notwithstanding, many practices may be eager to collect telehealth revenue immediately from patients rather than wait for insurance companies to pay, said Sabrina Corlette, a research professor and co-director of the Center on Health Insurance Reforms at Georgetown University. “Many employer plans are eliminating cost sharing” now that federal regulators have eased the rules for certain kinds of plans to improve telehealth benefits, said Brian Marcotte, CEO of the Business Group on Health, a coalition of very large, mostly self-insured employers.įor many doctors, business and billings have plunged because of the coronavirus shutdown.
Do telehealth visits have copays upgrade#
Nor can governors or state insurance regulators force those plans, which are regulated federally, to upgrade telehealth coverage. All four insurance giants say improved telehealth benefits don’t necessarily apply to such coverage. Such plans cover more than 100 million Americans - more than the number of beneficiaries covered by the Medicare program for seniors or by Medicaid for low-income families. Another is that Blue Cross Blue Shield, Aetna, Cigna, UnitedHealthcare and other carriers promoting telehealth have little power to change telemedicine benefits for self-insured employers whose claims they process. One problem is that insurers have waived copays and other telehealth cost sharing for in-network doctors only. “A lot of the insurers who said that they’re not going to charge copayments for telemedicine ― they haven’t implemented that,” said George Favvas, CEO of Circle Medical, a San Francisco company that delivers family medicine and other primary care via livestream.
Do telehealth visits have copays update#
Executives at telehealth organizations say insurers have been slow to update their software and policies. Patients say doctors and insurers are charging them upfront for video appointments and phone calls, not just copays but sometimes the entire cost of the visit, even if it’s covered by insurance.ĭespite what politicians have promised, insurers said they were not able to immediately eliminate telehealth copays for millions of members who carry their cards but receive coverage through self-insured employers.
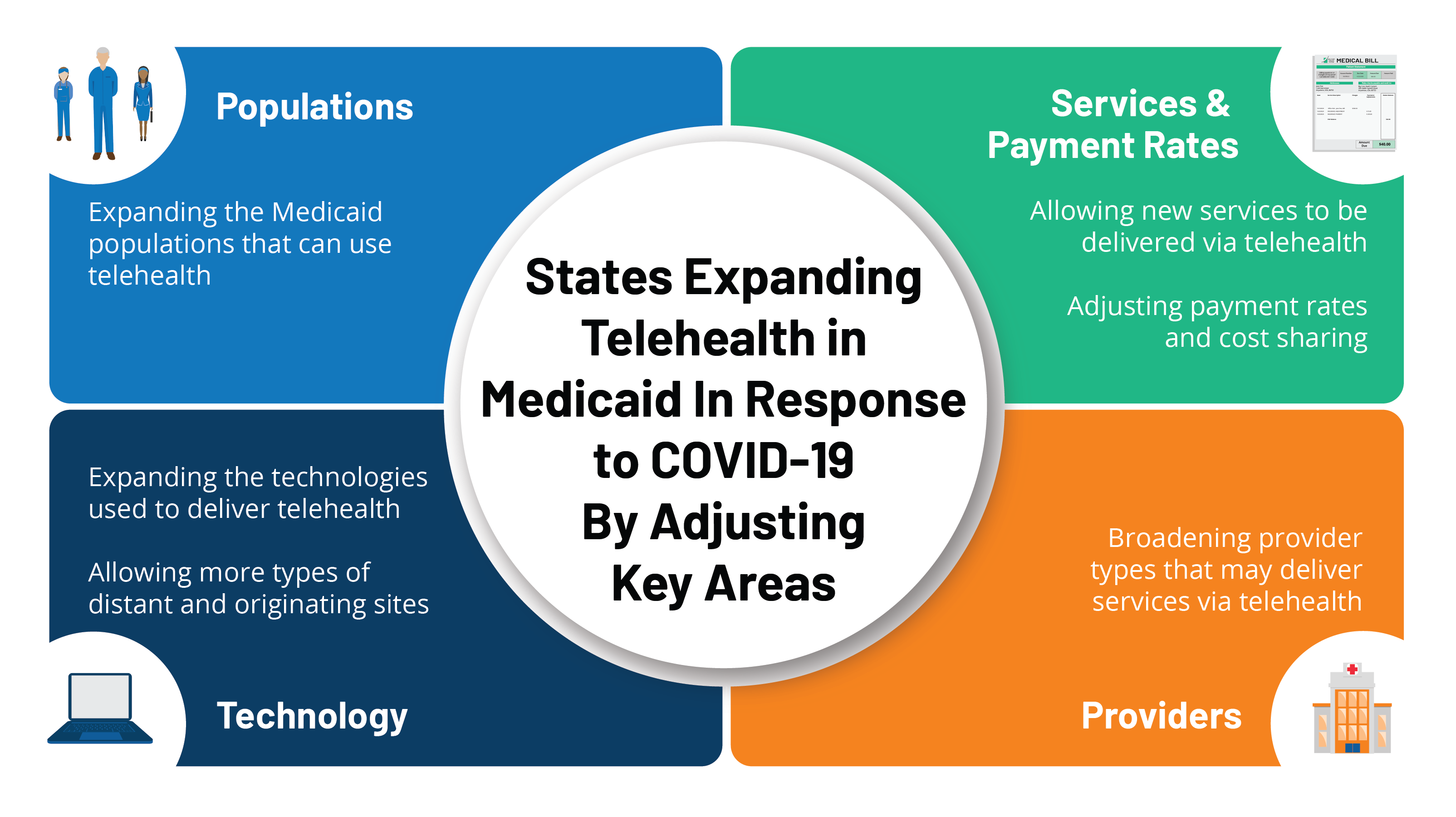
In some cases, doctors are billing for telephone calls that used to be free. Andrew Cuomo said last month after ordering insurers to eliminate copays, typically collected at the time of a doctor visit, for telehealth visits.īut in a fragmented health system - which encompasses dozens of insurers, 50 state regulators and thousands of independent doctor practices ― the shift to cost-free telemedicine for patients is going far less smoothly than the speeches and press releases suggest. “We are encouraging people to use telemedicine,” New York Gov. Policymakers and insurers across the country say they are eliminating copayments, deductibles and other barriers to telemedicine for patients confined at home who need a doctor for any reason.
Do telehealth visits have copays free#
Subscribe to KFF Health News' free Weekly Edition newsletter.


 0 kommentar(er)
0 kommentar(er)
